
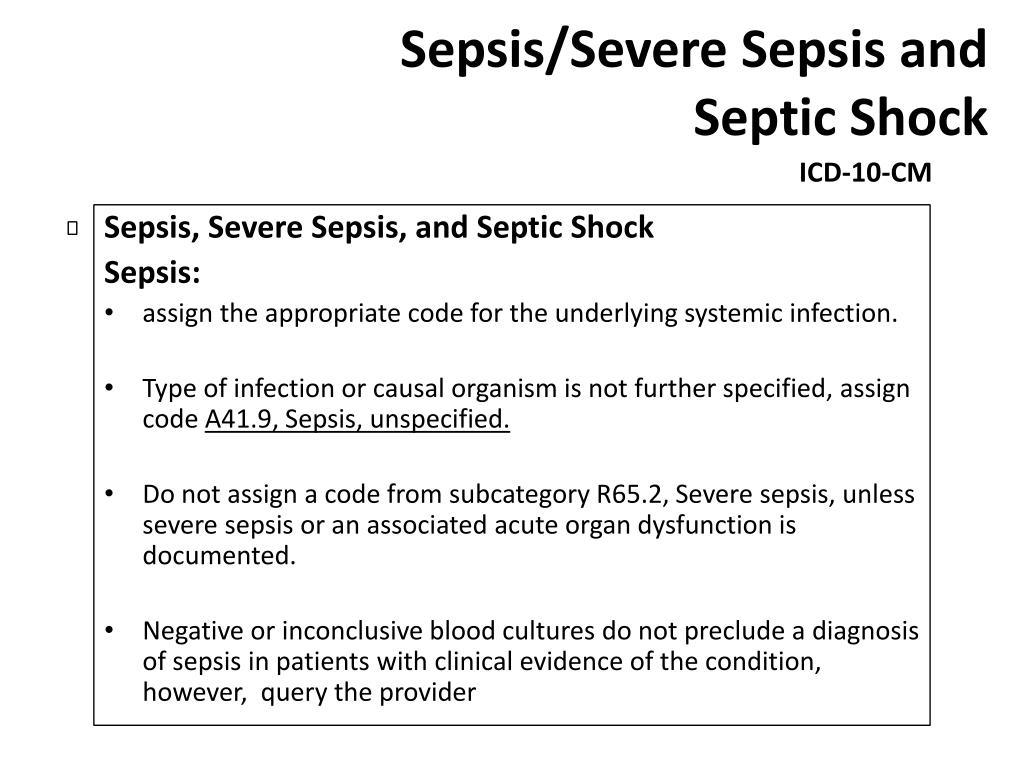
If the blood culture is negative or inconclusive, as this does not rule out the presence of sepsis.ICD-10 guidelines state that the coder should query the provider in the following instances:

One combination code is used to capture the underlying systemic infection and the body’s inflammatory response to it. For a diagnosis of sepsis, the appropriate code for the underlying systemic infection should be assigned, for instance, A41.51 (Sepsis due to Escherichia coli).If the underlying infection or causative organism is not further specified, code A41.9, Sepsis unspecified organism should be assigned.
Complete and accurate coding of severe sepsis, however, requires a combination of at least two codes – the first code sequenced to identify the underlying organism (Sepsis, A40.0 – A41.9) or cause of the sepsis (postprocedural infection, trauma, or burn), followed by a code indicating the extent to which the septic condition has progressed, that is, severe sepsis with or without septic shock. Since ICD-10 utilizes combination coding, sepsis without acute organ failure requires only one code, that is, the code for the underlying systemic infection (A40.0 – A41.9). Physicians should use the term “bacteremia” if there is evidence of bacteria circulating in the blood. While ICD-9 had codes whose description included the word “septicemia,” there is no code for septicemia in ICD-10. Experienced coders carefully review ICD-10 guidelines and clinical documentation to assign the right codes for sepsis, severe sepsis and septic shock. Coding of Sepsis and Severe Sepsis can be complicated and physicians would do well to rely on medical coding services to report these conditions. Sepsis is a life-threatening complication that develops when the chemicals the immune system releases into the bloodstream to fight an infection cause inflammation throughout the body instead.


 0 kommentar(er)
0 kommentar(er)
